Category: Latest
The electric light did not come from the continuous improvement of candles…
…Is a wonderful quote from the late professor and author Oren Harari.
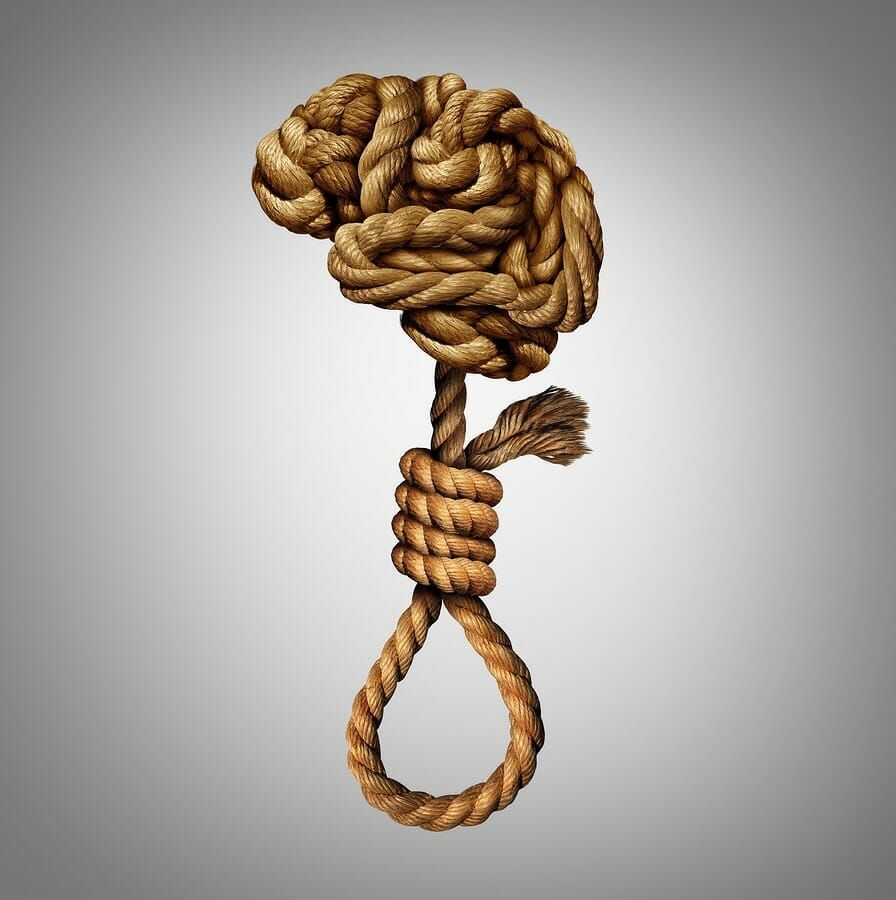
Considering the endless suicides, harrowing stories of mental anguish, woeful news reports lamenting the über-strained NHS, it’s easy to be pessimistic about the future of those enduring psychological crisis across the UK.
‘We’re spending more!’ – is the endless mantra of successive governments who don’t know what else to do.
‘We need more money to raise awareness!’ – is the mantra of mental health charities who don’t know what else to do.
‘We need to talk more!’ – is the mantra of employers who don’t know what else to do.
‘We need to tackle stigma!’ – is the mantra of psychiatry ‘experts’ who choose to blame stigma for the obvious lack of faith in the ‘therapies’ they provide.
On a deeper level,
and perhaps more insidious, is the prospect that psychiatry is in the habit of victim blaming in order to disguise their own charlatanism.
The more suicides there are, the more ‘awareness’ we are told we need to raise.
How much more ‘aware’ do we need to be before we become aware that despite the range of treatments available on the NHS, people are still killing themselves!
Let’s examine for a moment…
More awareness = more talking? = less stigma? = more accessing services? = improvement in mental health? = less suicides?.
Seems easy enough, but unfortunately, not many decision-makers want to see the elephant in the room – that the vast majority of those who have taken the ultimate path to peace after suffering a PTSD diagnosis, have indeed been in the hands of UK psychiatry, have accessed NHS services, and the ‘therapies’ approved by the National Institute for Health and Clinical Excellence (NICE).
Yet they still kill themselves, or descend into awful comorbidity, such as alcoholism, drug abuse, homelessness, and exploitation.
So why aren’t we questioning more the effectiveness of the ‘therapies’ on offer?
Why are we not questioning the evidence-base, and theoretical underpinnings for such treatment as ‘Eye Movement Desensitisation and Reprocessing’ (EMDR) for example, which is widely available across the NHS as a ‘treatment’ for posttraumatic stress?
-If you’re unaware how EMDR was developed, look it up – it was a psychotherapist called Francine Shapiro who, during a walk in a park one day, (apparently) ‘noticed’ that her eye movements reduced the intensity of disturbing thought she was having at the time.
The rest is history, and the training industry around EMDR has reached massive heights.
It is upon this amazing, coincidental and lucky(?) experience of Shapiros’ that the supposed experts who sit on the NICE PTSD committee decided to adopt EMDR, despite its dubious birth, lack of theoretical underpinning, and despite the fact that prior to Shapiros’ lucky thought, there had been no observed evidence that could or would have suggested a connection between the physical movement of an eye, the symptoms of PTSD, and (according to its proponents) the neurological systems of the brain.
A truly ‘Newtonian’ moment if ever there was one!
…except that gravity was observable, and the falling apple showed it – nor was Newtons’ the first apple that anyone had seen fall from a tree. Oh, and Newton didn’t sell the apple afterwards…
The same experts that languish in the corridors of NICE , and decide upon which ‘treatment’ the plebs get for PTSD, are (apparently) the leading scientists in the field – shame then, that they seem so busy in those corridors – it prevents them from carrying out any meaningful research into the issue that they label as PTSD.
Indeed, the leading lights of NICE psychiatry don’t seem to have either the will nor energy to carry out research that might actually prove helpful to mankind, and It’s often the case that the only ‘research’ they like put their names to are designed only to support their own trauma-based risk management systems that they peddle to unknowing but well-meaning employers.
And so, in closing, and returning to Hararis’ quote – how do we expect the effectiveness of trauma interventions to develop, when our foremost ‘experts’ are continually allowed to improve only their own candles?
It’s time for a new paradigm.
It’s time for science to robustly investigate trauma theory, and it’s time for a credible and ethical approach to decision-making within the committee that decides upon what ‘treatment’ they allow, and poignantly, how they justify withholding treatments that have a far greater evidence-base than those they currently endorse.
Business continuity, trauma, and recognising the new threat…
Many of us are familiar with ‘business continuity’ – threat analysis, business impact analysis, solution design (and testing) are now considered key to maintaining systems and services during periods of high threat such as spate conditions, direct, or indirect attack or strain.
Quite how these concepts transpose into the realm of mental health, however, is seemingly a mystery for many organisations.
Let’s consider for a moment some key components of a robust & systematic psychological continuity strategy that would enable your organisation to function effectively through, and in the aftermath of a critical Incident: