A truly person-centred, and highly effective approach to #PTSD #Stress and #anxiety #87RT
There are many therapists and counsellors that claim to be ‘person-centred’ in their approach, but how do people in distress even begin to understand what that actually means?
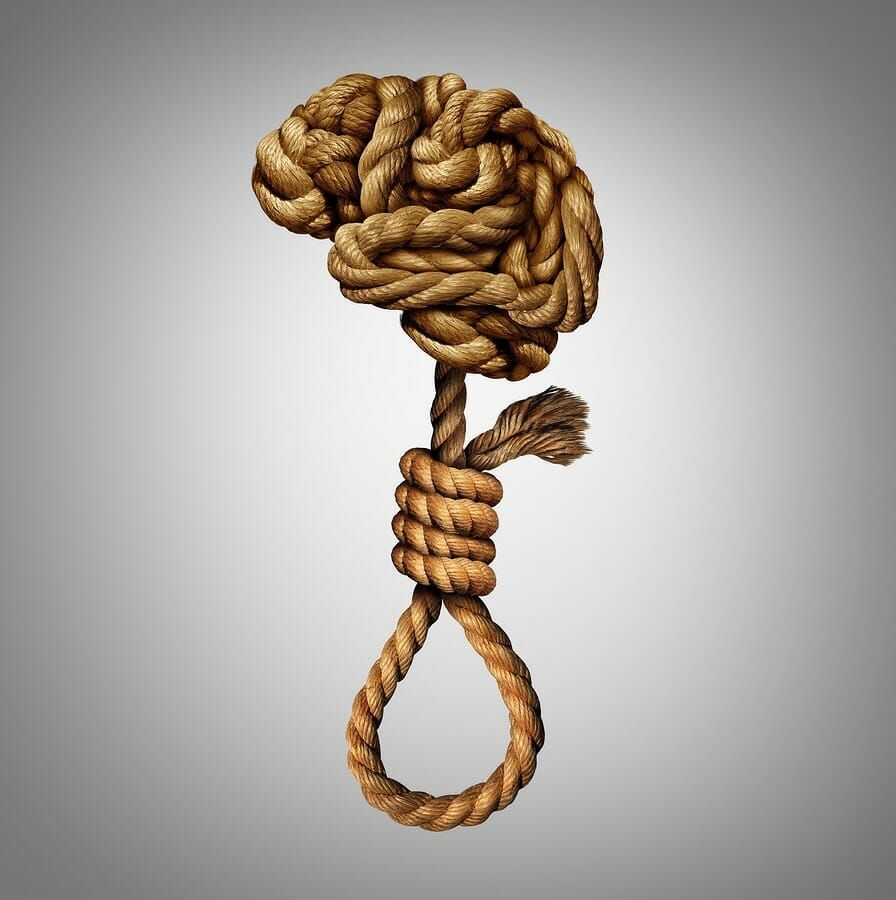
To many, the all-comsuming anguish they are enduring is paramount, and all they want is recovery. Recovery at all costs. Recovery from nightmares, recovery from flashbacks, and an end to panic attacks and the debilitating nausea and fear.
To whom do they turn when they cannot endure it any longer? Why, the experts – of course!
At this point, does the individual really have any interest in what is person-centred and what is not? I think it’s debatable at the point of crisis, but it is clear that it is at this very point that many ‘therapeutic’ relationships are damaged to the point where recovery cannot then even be a subsequence.
I cannot help but think that being ‘person-centred’ is merely the latest in a line of buzz words for many within the mental health sector, with little in the way of actual substance beneath the veneer. For in order to be truly person-centred, then we must eradicate judgement and interpretation – skills which are important within the clinical domain, through which most mental health ‘treatments’ are pipelined. I’ve seen being person-centred described as being ‘responsive to the wishes of the client’ – when all the clients wish for is to get better, then a natural void is formed into which steps the expert, and their opinion(s).
When dealing with someone in crisis, we have to be mindful that our conduct, attitude, and systematic approach are the most important factors in order for the individual to achieve recovery. This may sound self-evident as you read, but it is something that has been lacking within the clinical approach to mental health for years.
Many of our clients have already been through a normative therapy and counselling route, prior to their engagement with Social Support Systems. They’re often in crisis by that time, and we regularly hear stories of how they’ve felt failed, and worse, judged, by their previous counsellors, therapists, and the mental health system in general.
I remember one client telling me (during her initial consultation) that if I tilted my head to one side and appeared to feel sorry for her at any point, she would get up and walk out – she was so sick of being made to feel an object of pity, that her trust in mental health service providers was now somewhat nil.
What is often described as the ‘therapeutic relationship’ can clearly then have an affect upon the outcome of any recovery pathway, though that does not rest solely upon the professional standards, competence and the experience of the ‘expert’.
Crucially, the event of two individuals sitting together, is an act of communion. It is an act of communication.
When one of the individuals present is an ‘expert’, or perhaps (more importantly) considers themselves so, then naturally and consequently that communal relationship is not balanced. This is the very first challenge of the person-centred approach – the client is the underdog. They are needy due to crisis, and they are unknowing due to their lack of qualification. They are not the equal of the ‘expert’ sat before them.
Social Support Systems facilitators do not consider themselves to be the expert of anyone’s experiences. We know that the expert of experience, is s/he that had the experience.
After all, to claim some form of expertise by applying interpretation can serve only to augment the initial imbalance within the communion. Indeed, our facilitator’s first task is to restore equality to the relationship, and this is achieved by strictly adhering to our rules of facilitation.
In this manner, we achieve a thoroughly non-judgemental and safe environment in which people can consider themselves important within the process, and able to talk about their concerns free from the fear of interpretation and it’s consequences.
In such an environment, it then becomes not only possible but much easier for the client to talk about the unspeakable. A far more trusting relationship is developed, and It is in this fashion that we can, and do, enable an individual to reach into their darkest depths, and reveal the thing that they’ve dreaded for so long…
This is the true nature of being ‘person-centred’, and i’m convinced there is no better way of helping people in crisis through poor mental health.
To find out more about our person-centred work, or how we can help you or your organisation please contact us using the form below.
Best,
Sean McCallum
[contact-form to=”enquiries@socialsupportsystems.com” subject=”Enquiry from website”][contact-field label=”Name” type=”name” required=”1″][contact-field label=”Email” type=”email” required=”1″][contact-field label=”Message” type=”textarea”][/contact-form]